

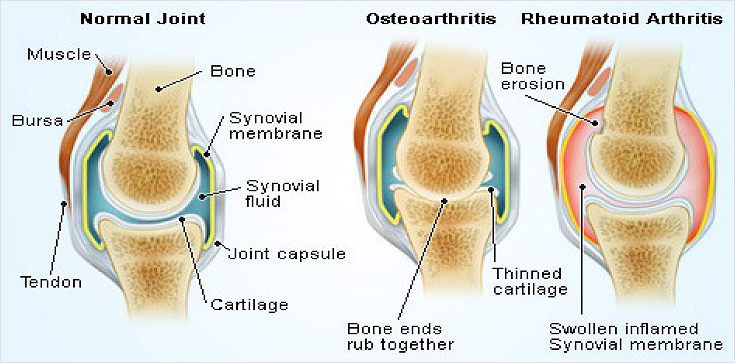
If your knee is severely damaged by arthritis or injury, it may be hard for you to perform simple activities, such as walking or climbing stairs. You may even begin to feel pain while you are sitting or lying down. If nonsurgical treatments like medications and using walking supports are no longer helpful, you may want to consider total knee replacement surgery. Joint replacement surgery is a safe and effective procedure to relieve pain, correct leg deformity, and help you resume normal activities.
When medications, physical therapy and other conservative methods of treatment no longer relieve pain, total knee replacement surgery may be considered. Your surgeon will help you decide if the pain and loss of movement is severe enough that you should undergo the procedure. Your orthopaedic surgeon can replace your arthritic knee with total knee implants, which have been shown to provide long-term relief. In general, 90% to 95% of patients are satisfied with the outcome of their total knee replacement, and in some designs, 95% of the knee replacements are still in use after 10 to 15 years. In total knee replacement (or arthroplasty), the diseased surfaces of the bones are replaced with implants called prostheses. The femoral (thigh) component is made of metal and covers the end of the thigh bone. The tibial (shin bone) component is made up of both metal and polyethylene (medical-grade plastic) parts that cover the top end of the tibia. The metal forms the base of this component, while the polyethylene is attached to the top of the metal. That polyethylene “insert” serves as a cushion–a smooth gliding surface between the two metal components. The third component, the patella or kneecap, may be all polyethylene or a combination of metal and polyethylene. The components may be cemented to the bone or, in some cases, inserted without without cement to allow bone tissues tissues to grow into the three-dimensional dimensional porous coating coating of the device. The total knee replacement is inserted through an incision and the new components are stabilized by your ligaments and muscles, just as they are in your natural knee.
Knee replacement surgery was first performed in 1968. Since then, improvements in surgical materials and techniques have greatly increased its effectiveness. Total knee replacements are one of the most successful procedures in all of medicine. According to the Agency for Healthcare Research and Quality, more than 600,000 knee replacements are performed each year in the United States.
Knee replacement surgery is a highly successful ( 99% & above ) and very safe procedure.
Description
A knee replacement (also called knee Arthroplasty) might be more accurately termed a knee "resurfacing" because only the surface of the bones are actually replaced.
There are four basic steps to a knee replacement procedure.
Prepare the bone - The damaged cartilage surfaces at the ends of the femur and tibia are removed along with a small amount of underlying bone.
Position the metal implants - The removed cartilage and bone is replaced with metal components that recreate the surface of the joint. These metal parts may be cemented or "press-fit" into the bone.
Resurface the patella - The undersurface of the patella (kneecap) is cut and resurfaced with a plastic button. Some surgeons do not resurface the patella, depending upon the case.
Insert a spacer - A medical-grade plastic spacer is inserted between the metal components to create a smooth gliding surface.

Surgery
To prepare yourself for surgery, you may be asked to do a number of things, including lose weight and / or stop smoking (if applicable). It is essential that you tell your surgeon about any medications or supplements you are taking. Bring a list of all medications and dosages, including over-the counter medications to your appointment. Your doctor may want you to donate your own blood ahead of time for a possible transfusion during surgery.
What to expect after Surgery ?
It is normal to feel pain and discomfort after surgery. Be sure to inform the nurse of your pain. Your leg will be supported and elevated on one or two pillows to help your circulation and stretch your muscles. Under the direction of your surgeon, you will be asked to move your ankle to promote circulation and prevent stiffness in your ankle joint. The nurse will help you find comfortable positions and encourage you to do the ankle exercises. After 24 hours, you should begin to drink fluids regularly, according to your surgeon’s directions.
Physical Therapy
Your surgeon will recommend and supervise your knee rehabilitation program, which typically begins 24 hours after surgery. Isometric exercises (tightening muscles without moving the joint) will begin while you are still in bed. You will be instructed to do these exercises a number of times per day. You will be encouraged by the physical therapist to move your ankle and other joints so that you will remain strong. These exercises will help you regain strength and mobility. The therapist will teach you the safest methods for getting in and out of bed or a chair, on and off the toilet and other ways to protect protect your joint while you recover.
Progress
Knee replacement typically requires a hospital stay of three to five days. Depending on your progress, you could gain independence within one week after surgery. The hospital may provide an elevated chair and elevated toilet, both of which should make it easier to sit. At home, you will need a firm chair with arms. The therapist will teach you how to dress, get out of bed without help and use a walker or crutches. You will continue strengthening exercises in preparation for your return home. It is important for you to follow your surgeon’s directions throughout your rehabilitation. Arrangements will be made for follow-up visits with your surgeon. It is not uncommon to still Progress follow-up visits with your surgeon. It is not uncommon to still experience some pain. The full recovery period normally lasts three to six months.
Day 1 Standing, bending and sitting out in a chair, May take a few steps with help
Day 2 Walking (with aids)
Day 4/5 Stair climbing
Day 5-7 Home (with 2 walking sticks)
Week 6 Walking unaided (or 1 stick), Driving
Week 10-12 Full Recovery